5 Steps to Creating Effective Community Health Initiatives

Hospitals around the country are leaning in to address patients’ social determinants of health. As they develop community benefit programs to address health disparities and elevate community well-being, co-investment with like-minded partners helps drive greater impact.
But, perhaps what is still not clearly defined is how to go from idea to implementation.
Community benefit managers and C-suite leaders alike struggle with questions: Where do we start? Who should be involved in the planning process? How do we develop sustainable funding for community health programing? And with a goal as ambitious and nebulous as elevating community well-being, how do we evaluate success?
In this post, we will explore some of the major steps to creating effective community health initiatives, and share one case study.
1. Start with the data to define your position in the market and create a high-impact community benefit program that promotes equity.
Your Community Health Needs Assessment (CHNA) has a wealth of information. What are other organizations doing in this space? Look for that unique opportunity in the space that gives you an innovative, authentic way to help.
Tip: Health care systems can align their existing community benefit budgets by directly investing in the top CHNA priority area. Create a master community benefit cost center across the system so that financial transactions can be tracked and shared in real time. One cost center promotes one mission and eliminates spending in silos. A master community benefit cost center also makes end of year financial reporting easier, such as completing a Schedule H.
2. Consider the “WHY.”
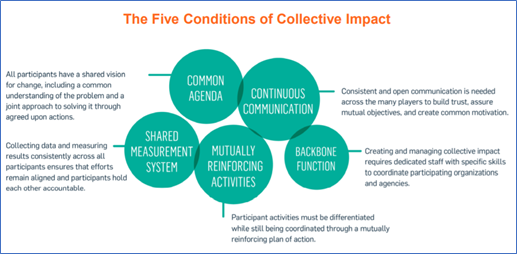
Why do you want to play a role in addressing this social issue? How is your organization positioned to help in a given space—say, the bridge between housing and health? Start with purpose and develop your framework from there. A public health tool framing collective impact can allow you to create the vision of why, how, and with whom.
Tip: Get colleagues to buy into your “why” early on and create a small working group. Involving a diverse set of experts early in the process allows you to get “weight” for your concept and creates a sense of excitement for building the case for change. Remember to include community-based experts.
3. Look outside the box for funding partners.
Hospitals cannot solve these issues in a silo. And, just as health systems seek to serve as change agents, many corporate partners are looking to align their social impact funding in a way that can have a measurable impact and help them to live out their values. Identify like-minded partners with the mission, funding, and resources to help you grow the program’s reach. Invite your development colleagues to the table early in the process; they may have funders in mind that could be an excellent match.
4. Be accountable to your internal and external stakeholders.
It is your job not only to create the best possible program, but to seek regular input and to communicate the wins and challenges along the way. Collaborating with community-based organizations (CBOs) not only strengthens your collective efforts, but helps the community you serve to buy into your program and vision.
5. Get your Board on board.
You may be fortunate enough to already have CEO support. If not, you must relentlessly share your “community health story” with the C-suite and Board. Trustees have an important role to play in guiding the hospital’s trajectory by balancing different essential priorities. With proper communications, data sharing, and mission anchoring, obtaining Board buy-in is possible. Further, pitching a new program with partner funding underscores that the community sees a pressing need.
Case Study: Inspira Health Network and Partners Tackle Pediatric Obesity
Obesity and food insecurity are intertwined. Furthermore, food-insecure individuals are 50% more likely to experience Type 2 diabetes and 60% more likely to experience heart disease. In 2019, the Robert Wood Johnson Foundation released their County Health Rankings Report. Salem and Cumberland Counties were last in health outcomes and health behaviors. This statistic was reaffirmed in Inspira Health Network’s recent CHNA. Inspira closely examined their data and discovered that children ages 10-17 were experiencing double the rate of obesity of anywhere else in New Jersey. This became their “why.”
While Inspira was developing its community health strategy, the Inspira Foundation was sharing this new direction with potential partners. TD Bank made a leadership gift of $500,000 to help catalyze a program that would address the social risk factors Cumberland and Salem’s children were experiencing.
Inspira launched two “Food Farmacy” programs to promote access to healthy foods and nutrition education to patients screening positive for obesity or food insecurity in the primary care setting and Emergency Department. Critically, these programs also measure outcomes over time through Inspira’s electronic medical record.
Bolstered by the TD Bank gift and in partnership with local food banks, Inspira also took their approach beyond the hospital’s four walls and helped create a “Costco in a parking lot.” This program targets schools where there is a high rate of obesity and a high percentage of children enrolled in the free breakfast and lunch program.
The program’s goals are to reduce chronic disease burden over time by reducing food insecurity and promoting healthy food access. Inspira also provides fitness staff to facilitate gym assemblies on staying active. Families are able to come and “shop” for free once a month. A Registered Dietician is on site to talk with families about nutrition concerns. Additionally, Inspira deploys nutrition interns to conduct surveys of patients.
Program Success
There are many ways to measure program success. It is essential to gather good baseline data.
- Initial data: Nearly every baseline survey conducted in the program’s first month demonstrated that 70% of respondents screened for significant levels of food insecurity as well as moderate chronic disease.
- Each site receives a sponsorship from Inspira of $10,000 per school year, for a per-person benefit of $5.55 per month.
- Each family walks away with an average of 60 pounds of food for the month, including fresh dairy, fresh produce, meats, grains, and canned vegetables. The program also provides toiletries and household items like toilet paper.
- There is an average distribution of 7,000 pounds of food to 100+ families per month, per school site. These 100 families comprise approximately 400-500 individuals.
- Metrics include improved blood pressure, reduced blood sugar, and weight loss.


